for 42 years
Where do you have pain?Choose the department and find out treatment
-

Back·Pelvis·Leg
- Sprain
- Disc Bulging/Herniation
- Foraminal Disc Herniation
- Degenerative Disc Disease
- Spinal Stenosis
- Spondylolisthesis
-

Neck·Head·Shoulder·Arm
- Disc Bulging/Herniation
- Foraminal Stenosis
- Ossification of the Posterior Longitudinal Ligament
-
Middle Back·Flank
- Disc Bulging/Herniation
- Ossification of the Ligamentum Flavum
- Ossification of the Posterior Longitudinal Ligament
- Fracture
People who chose WooridulPatients and spine specialists from all over the world have visited Wooridul Spine Hospital
WOORIDUL
MEDICAL
EXCELLENCES

Minimally Invasive Spine Surgery and Causal Treatment
Wooridul Spine Hospital's original and unique surgical method which can preserve normal tissue through minimal incision and precisely treat the lesion only
In 1992, Wooridul Spine Hospital was established a new ‘endoscopic laser spine treatment’ combining laser with the existing endoscopic procedures, and opened the new era of minimal-incision spine surgery. For 40 years, we have been leading the global paradigm of the spine treatment by researching and developing the methods of minimal-incision treatment.
Find out moreWooridul is No.1 institution in the spine treatment field
Statistics prove it!
-

503,964
Spine Treatment Cases performed at Wooridul
2000~2024.03
-

25,378
International Patients treated at Wooridul
2006~2024.03
-

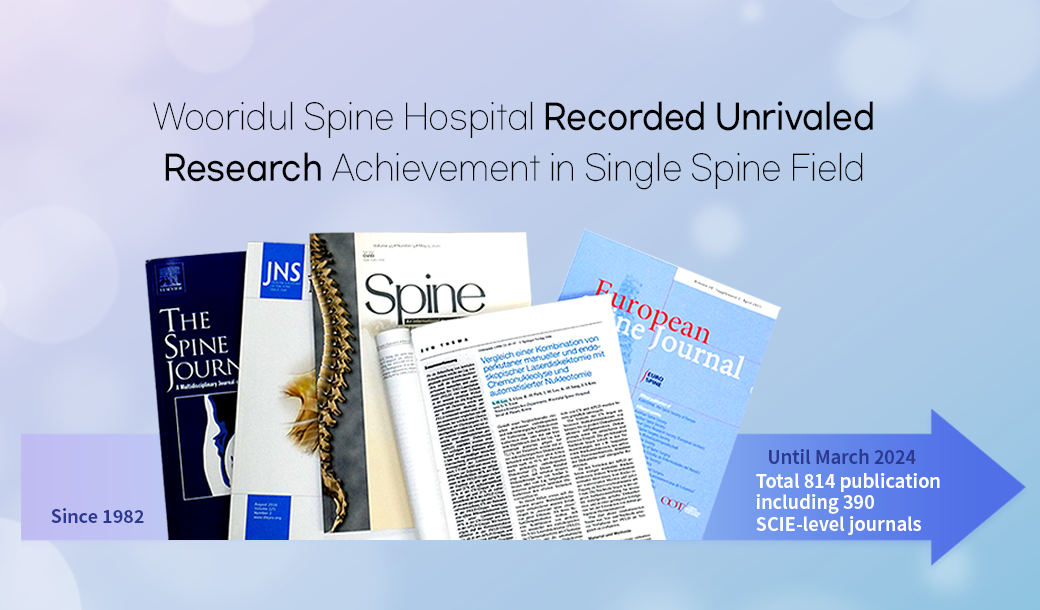
SCIE 390
Global Journals published by Wooridul
1982.03~2024.03
-

907
Foreign Doctors trained at Wooridul
1993~2024.03



































 Accreditation of Spine Specialty Hospital by the Korean Ministry of Health and Welfare
Accreditation of Spine Specialty Hospital by the Korean Ministry of Health and Welfare Healthcare Accreditation by the Korean Ministry of Health and Welfare
Healthcare Accreditation by the Korean Ministry of Health and Welfare Healthcare Provider Certification for International Patients by the Korean Ministry of Health and Welfare
Healthcare Provider Certification for International Patients by the Korean Ministry of Health and Welfare Top 10 World’s Best Hospitals for Medical Tourists
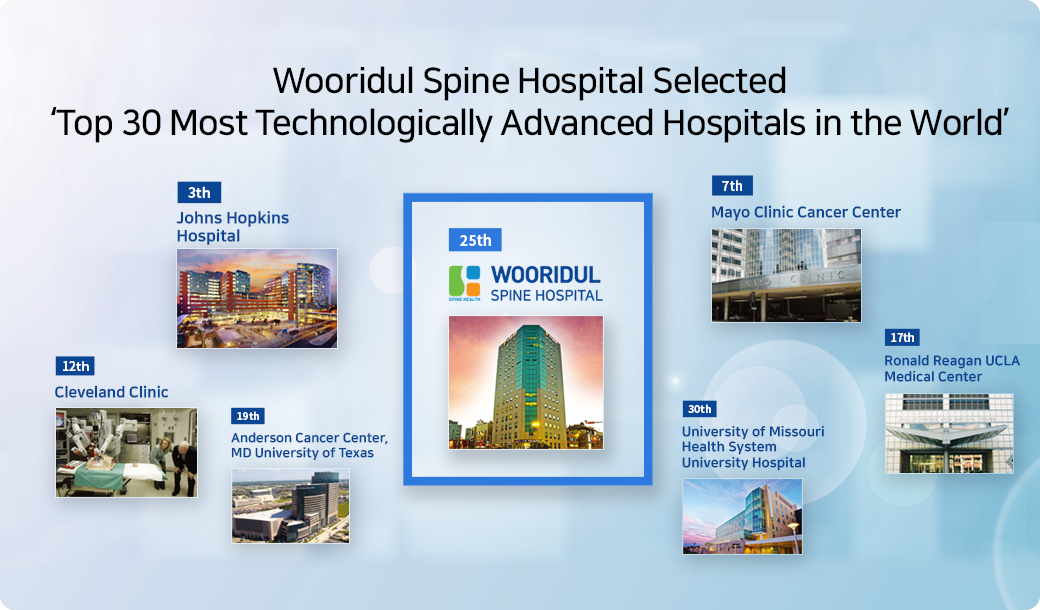
Top 10 World’s Best Hospitals for Medical Tourists 30 Most Technologically Advanced Hospitals in the World
30 Most Technologically Advanced Hospitals in the World The World’s Best Smart Spine Hospital 2024 selected by Newsweek
The World’s Best Smart Spine Hospital 2024 selected by Newsweek